Since its creation in 1965, Medicaid has helped millions of Americans gain access to healthcare. This federal and state program provides healthcare coverage to low-income Americans, children, people with disabilities, pregnant individuals, and elderly adults. While it is administered by states, it is funded jointly by states and the federal government.
Several studies have shown that Medicaid has positive health outcomes, by increasing access to healthcare services, specifically for low-income Americans. However, many still wonder – to what degree does the program help uninsured or underinsured Americans? And, what level of impact can it have on the general public? Luckily, Low Income Relief has already done this research for you.
How does Medicaid measure its results?
Each year, the Centers for Medicare & Medicaid Services (CMS) publishes an annual report to showcase which health outcomes were achieved for those participating in these programs. The CMS has separate indicators for children and adults, to show the differing impacts of the healthcare program on different populations. Most of these indicators include information such as immunization status, hospitalization statistics, number of ambulatory visits, and related figures.
However, the main metric that most policy makers and Americans are interested in is the enrollment number. Congress reports that since February 2020, Medicaid and CHIP (Children’s Health Insurance Program) enrollment has increased by an outstanding 23%, or by over 16 million. As of January 2022, 79,982,228 people were enrolled specifically in Medicaid. Due to the COVID-19 Pandemic and impending recession impacting the United States, enrollment figures continue to increase, as more Americans fall below the income threshold, making them eligible for government programs.
Since states administer Medicaid, they are also in charge of monitoring the system performance. However, this is mainly voluntary, and many states have not yet begun comprehensive monitoring and evaluation. The federal government recommends that states report in 8 different areas:
- Affordability and Efficiency
- Behavioral Health
- Chronic Conditions
- Equity
- Person-Centered Care
- Seamless Care Coordination
- Safety
- Wellness and Prevention
Are the results of Medicaid positive?
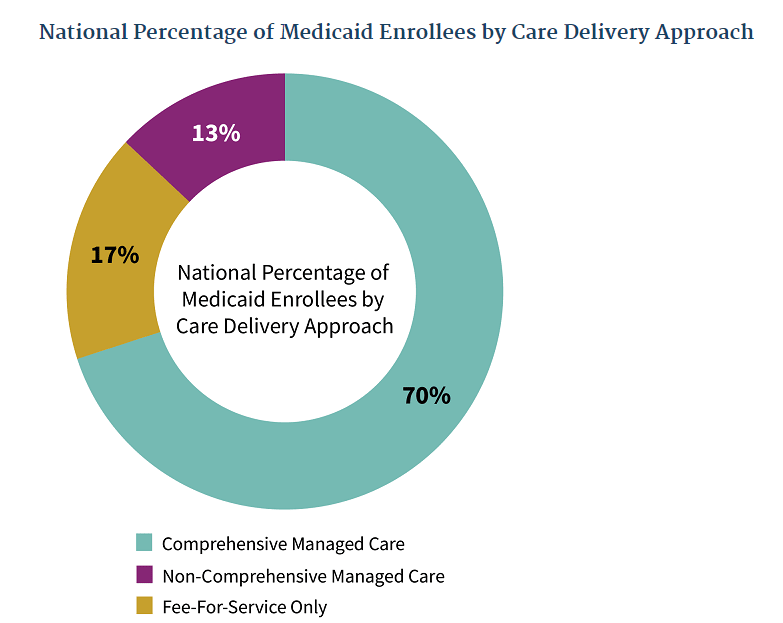
According to CMS, 70% of those enrolled in the program receive comprehensive managed care. This type of care is intended to better integrate the program into the healthcare system and provide better services to participants. This approach helps reduce healthcare costs and improve the management of health services, by contracting specific Medicaid agencies and managed care organizations (MCOs).
Since there are so many indicators to measure health, it can be difficult to see the overall effect of Medicaid on its participants. However, we have pulled some highlights below:
- Together, Medicaid and CHIP provide coverage for about 42% of births nationwide.
- In December 2020, Medicaid was expanded to include more low-income adults, leading to an additional 18,740,932 gaining access to healthcare.
- 49% of individuals enrolled in Medicaid are children.
How do other organizations view Medicaid’s results?
Under the 2010 Affordable Care Act, Medicaid programs were expanded, leading to many organizations to measure the program’s effectiveness.
According to the Kaiser Family Foundation, the expansion of Medicaid led to an increased access to care and an overall increased utilization of health services, particularly among low-income Americans. As a result, this has led to an increase in diagnosis of diseases and conditions, which can help prevent health complications later in life. For example, with the program’s expansion, there was increased access to certain types of cancer surgeries. Additionally, there was also a 24% increase in the use of a smoking-cessation medication, among program participants. Finally, there was also an 18% increase in admission to specialty treatment facilities for opioid addiction.
Other organizations are in agreement. The Robert Wood Johnson Foundation reports that since New York, Arizona, and Maine have expanded Medicaid, there was a 6 percent decrease in mortality rates among 20 to 64 year olds. As of 2019, there was also program expansion in Arkansas and Kentucky. Compared to Texas, where there was no expansion, program participants in these two states had a 23 percentage point difference to self-report a status of “excellent health.” They also had a higher chance, by 41 percentage points, to report a usual source of medical care. The Robert Wood Johnson Foundation emphasizes that expanding the program not only has positive health outcomes, but also economic outcomes, through the creation of jobs. In Louisiana, 19,200 jobs were created through the Affordable Care Act, and other states had similar results.
The Commonwealth Fund also reports that program expansion has successfully reduced uncompensated care burdens for patients and hospitals. In fact, “For each additional dollar spent on hospital services for Medicaid patients in expansion states, hospitals enjoyed an approximate 41-cent reduction in uncompensated care costs.”
What’s the difference between Medicaid and Medicare anyway?
Medicaid is considered a healthcare “assistance” program for low-income Americans of all ages. In other words, patients typically pay little to no cost for covered medical expenses, but a small co-payment may be required.
On the other hand, Medicare is a health “insurance” program, only available to people over 65 years old and people with certain disabilities. For this program, medical bills are paid through a federal trust fund, and patients may have to pay deductibles for hospital visits and related costs. While Medicaid is administered by states, Medicare is a purely federal program.
So, how much does Medicaid actually cost for patients?
Since Medicaid is administered separately by states, each state has the authority to charge premiums or charge other out of pocket costs. These out of pocket costs may include deductibles, copayments, and related costs, although children and pregnant women are typically exempt from these.
The federal government limits how much states can charge the following groups in premiums:
- Pregnant women and infants at or above 150% the federal poverty level
- Disabled individuals with income above 150% the federal poverty level
- Disabled children, deemed eligible according to the Family Opportunity Act
- Other medically needy individuals
In Conclusion
Ultimately, Medicaid is a valuable resource to more than 80 million Americans nationwide. If you think you may qualify for the program, Low Income Relief has prepared a comprehensive guide on how to apply. If you are looking to renew your Medicaid eligibility, it is important to do so promptly.